Powerful Features for Modern Healthcare Billing
Everything you need to streamline coding, reduce denials, and accelerate your revenue cycle.
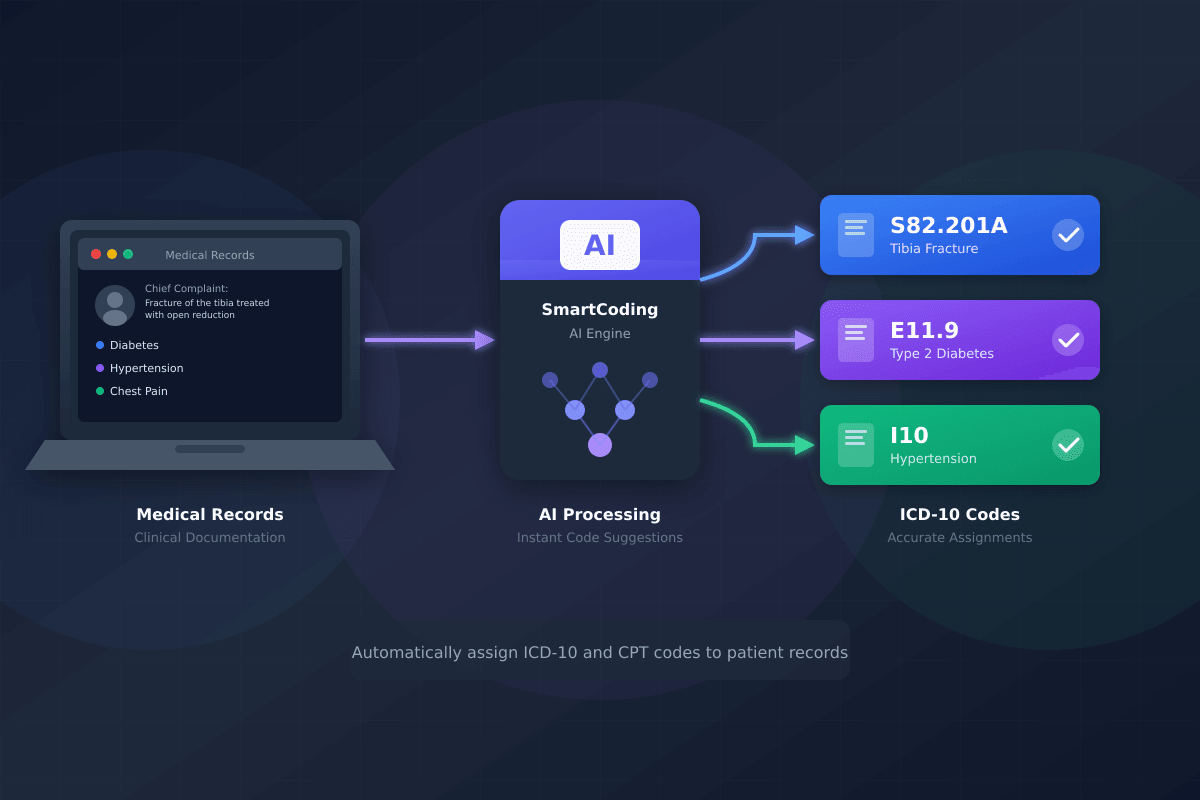
Let AI Handle the Heavy Lifting
Our advanced AI reads and understands clinical documentation, suggesting the most accurate ICD-10 diagnosis codes and CPT procedure codes in seconds—not minutes.
- Analyzes clinical notes in under 5 seconds
- Confidence scores for each suggested code
- Clear reasoning for every recommendation
- Supports all medical specialties
- Learns from your corrections over time
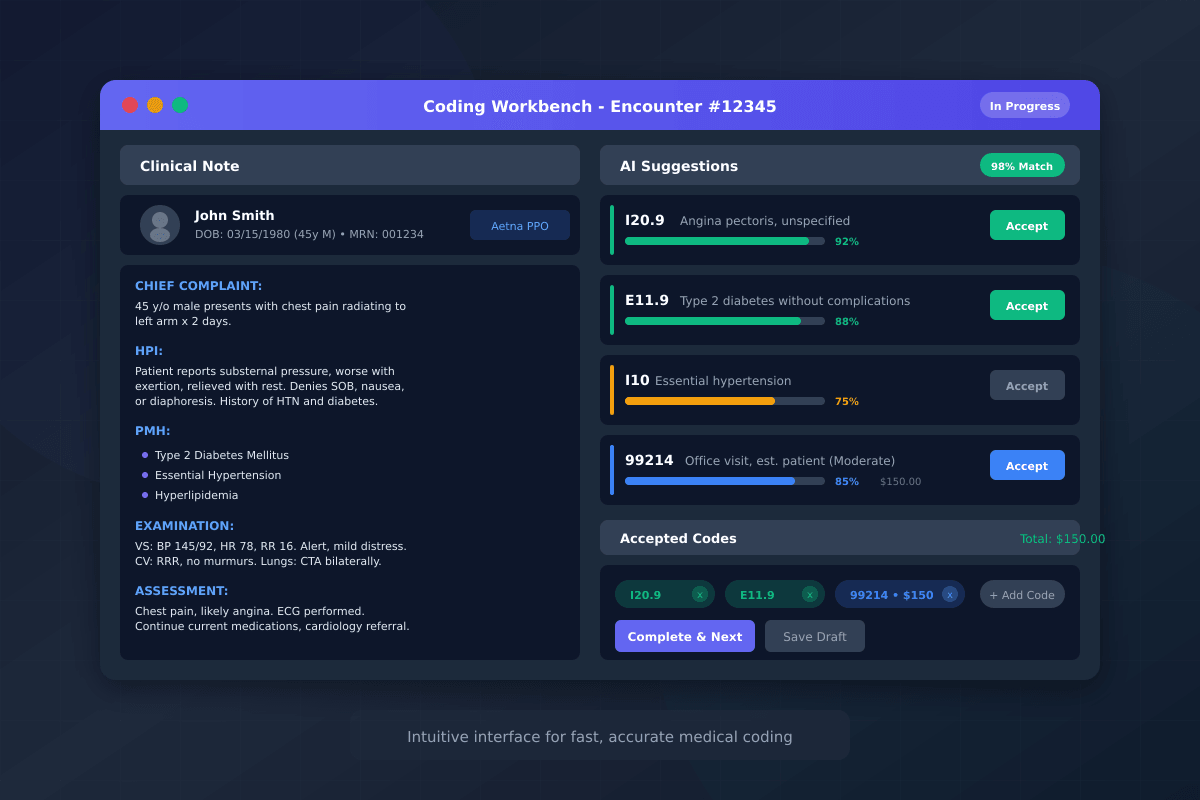
An Intuitive Interface Coders Love
Our coding workbench puts everything your team needs in one view—patient info, clinical note, AI suggestions, and accepted codes—all without switching screens.
- Split-screen view for maximum efficiency
- One-click accept or modify suggestions
- Intelligent code search with autocomplete
- Keyboard shortcuts for power users
- Auto-save draft functionality
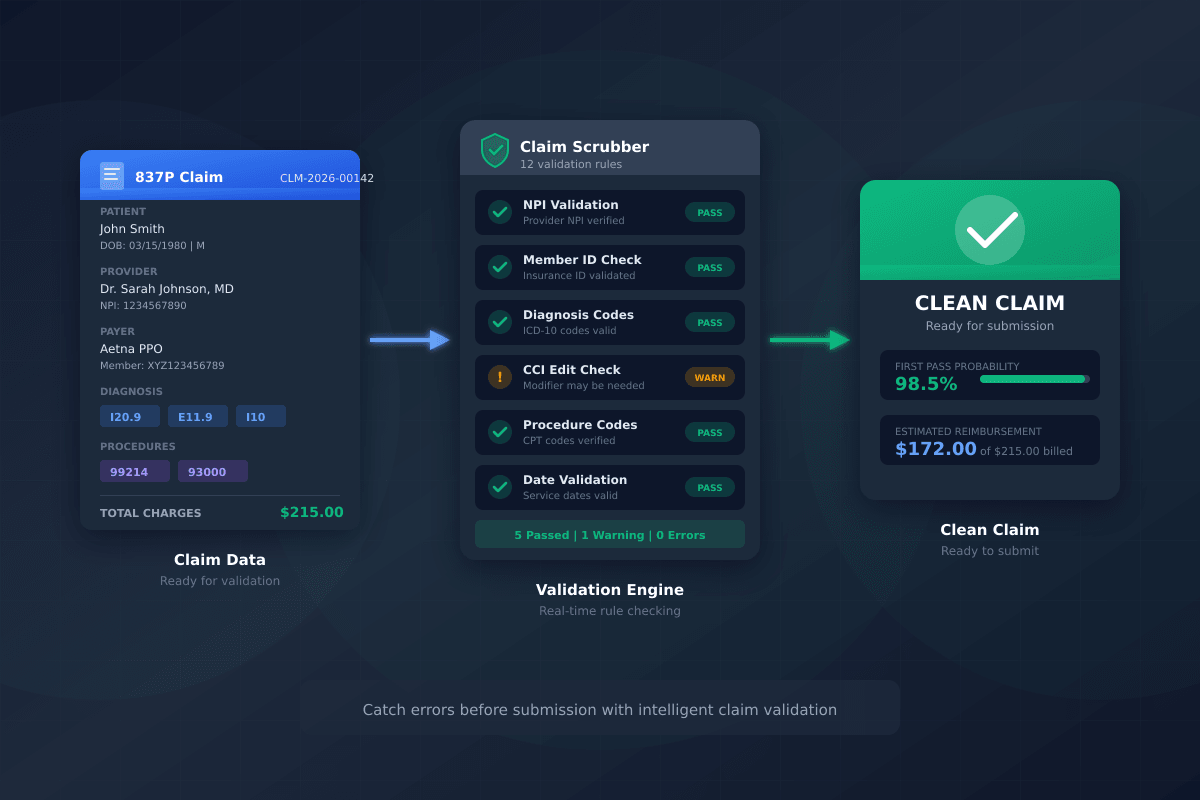
Catch Errors Before Payers Do
Our intelligent scrubbing engine validates every claim against thousands of rules before submission, dramatically reducing rejections and denials.
- CCI edit detection and alerts
- NPI and Tax ID validation
- Gender and age-specific code edits
- Payer-specific rule engines
- Missing information alerts
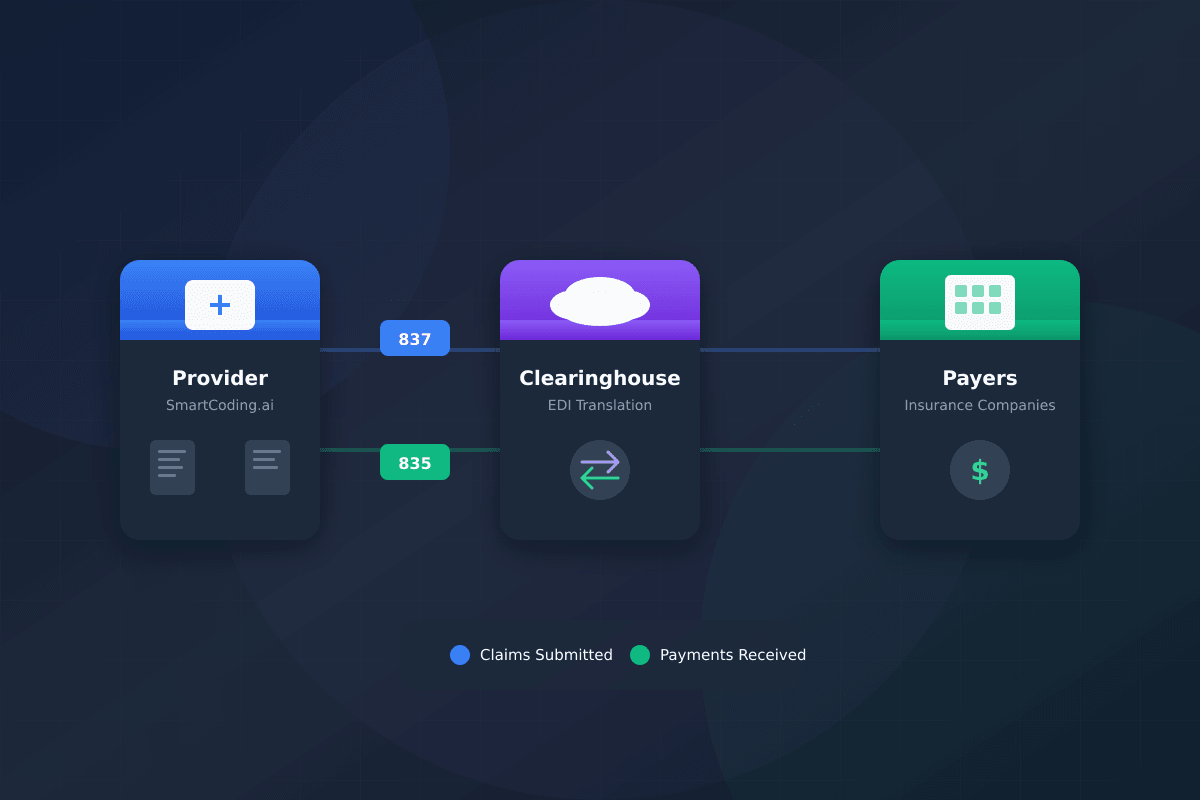
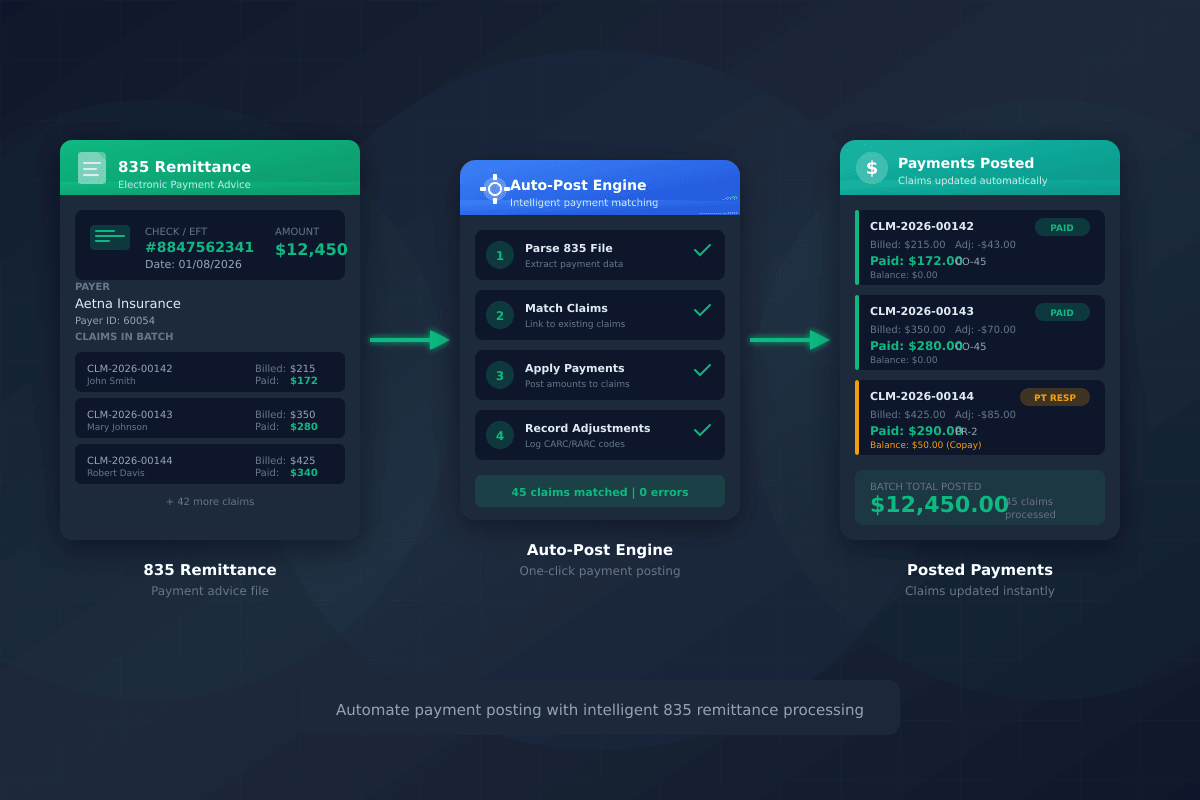
Seamless 837/835 Handling
Generate HIPAA-compliant 837P claims and automatically parse 835 remittance files. We speak the language of healthcare billing so you don't have to.
- HIPAA 5010 compliant 837P generation
- Automatic 835 parsing and matching
- Support for all major clearinghouses
- Real-time claim status tracking
- Batch and individual claim processing
Automatic Payment Reconciliation
Import 835 remittance files and watch payments automatically match to claims and post to your accounts. No more manual data entry nightmares.
- One-click 835 import and processing
- Smart claim matching algorithm
- CARC/RARC code interpretation
- Exception handling for unmatched payments
- Complete audit trail
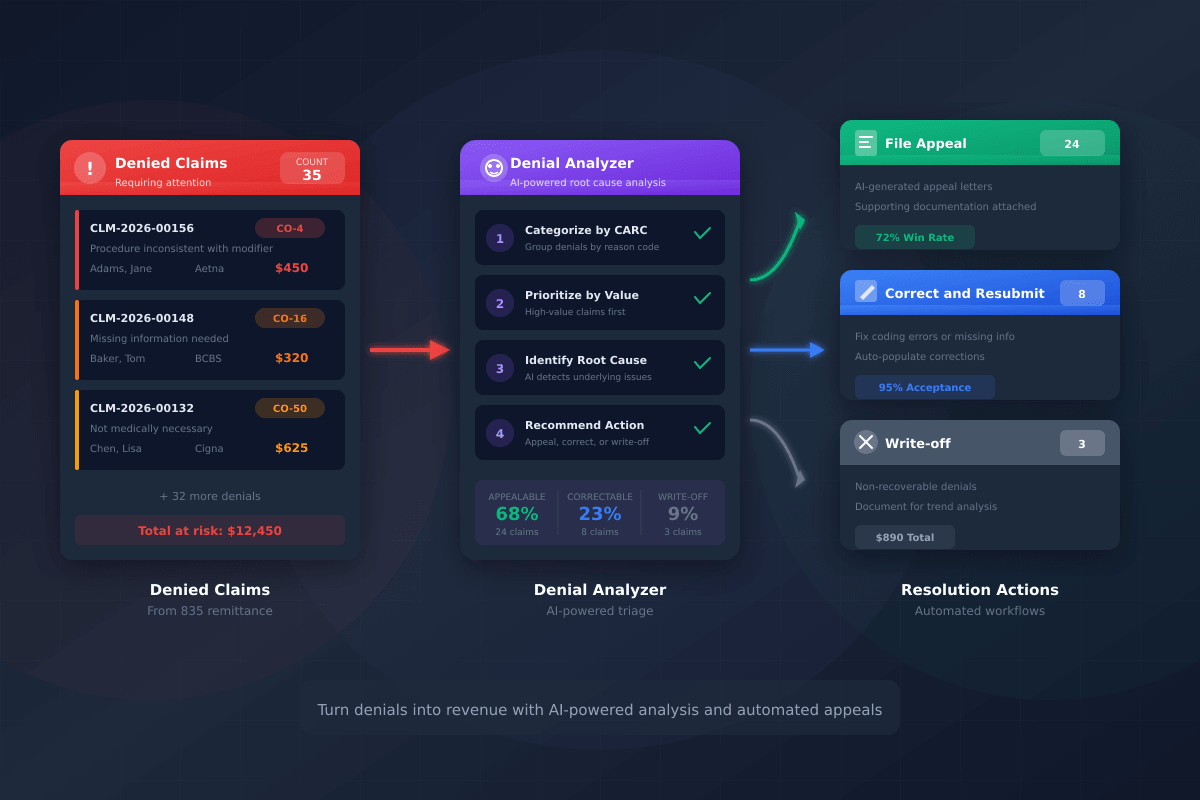
Turn Denials Into Revenue
Our denial worklist prioritizes high-value claims and helps your team resolve issues faster. AI-generated appeal letters save hours of manual work.
- Prioritized denial worklist by value
- Root cause analysis by CARC code
- AI-generated appeal letters
- Appeal tracking and follow-up
- Denial trend reporting
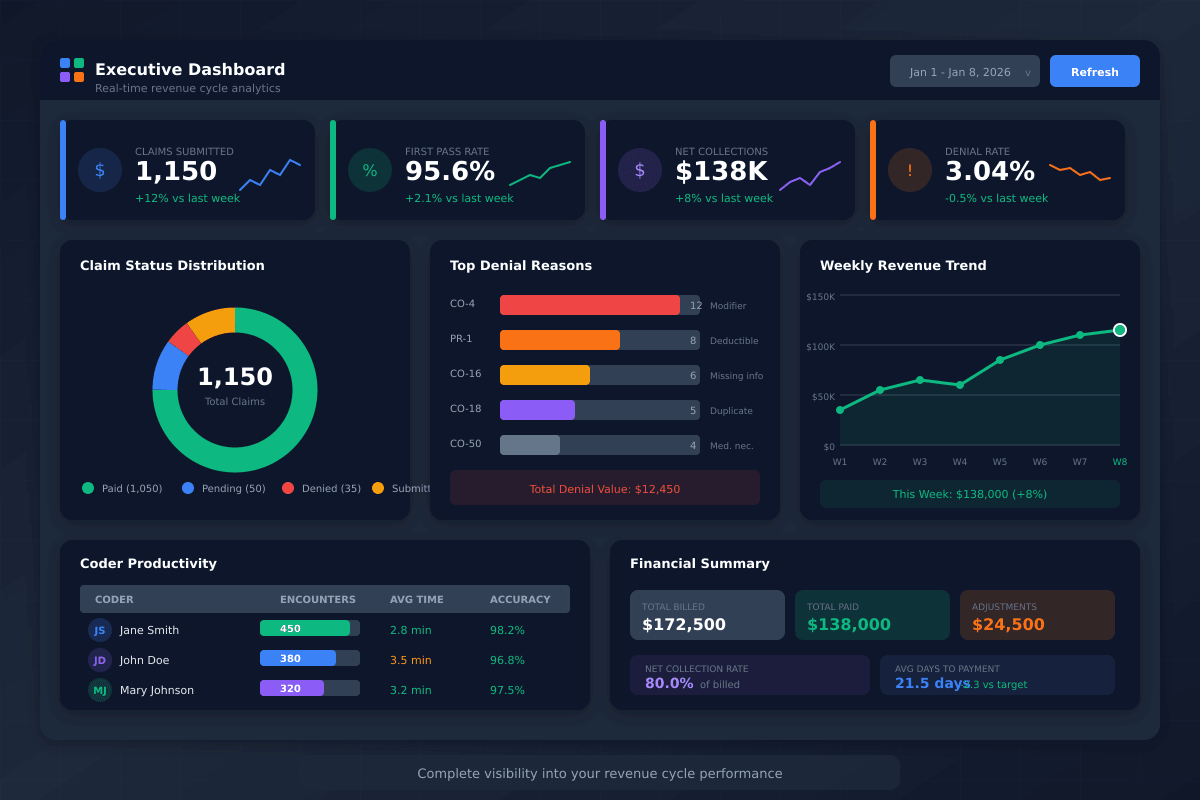
Insights That Drive Decisions
Real-time dashboards and customizable reports give you complete visibility into your revenue cycle performance. Know exactly where you stand, always.
- Executive dashboard with key KPIs
- Coder productivity metrics
- First pass rate tracking
- Denial rate analysis by payer/code
- Days in A/R trending
Works With Your Existing Systems
SmartCoding.ai integrates seamlessly with leading EMRs, practice management systems, and clearinghouses.
EMR Systems
Epic, Cerner, Athena, and more via HL7 and FHIR.
Clearinghouses
Availity, Change Healthcare, Trizetto, and others.
Practice Management
Major PM systems supported out of the box.
REST API
Full API access for custom integrations.
Ready to See These Features in Action?
Schedule a personalized demo and discover how SmartCoding.ai can transform your revenue cycle.
